Dr Alfi and his team in front of the Kobe Bryant mural in his clinic: a daily inspiration to “be the best version of yourself and continue to grow”

By Daniel Ramos
⋅ 4 min read
⋅ Updated Jul, 2024
In episode one of the Expand podcast, Dr Daniel Ramos was joined by oral and maxillofacial surgeon and private practice owner, Dr David Alfi from Los Angeles, California, to talk about all things airway. Among other topics, their must-listen discussion covered:
The concept of "The Quiet Pandemic," referring to the widespread issue of reduced jaw sizes and constricted airways in modern populations.
Interdisciplinary collaboration among specialists, including orthodontists, surgeons and other dental professionals, to address complex cases more effectively.
Advancements in surgical techniques, especially in jaw surgery, which have become less invasive and more predictable thanks to digital planning and custom surgical guides.
Read on for some of the highlights from this episode or listen to the conversation in full on Spotify, Apple Podcasts or YouTube.

The evolutionary shift towards smaller jaws
The conversation got off to a start with a discussion around the ‘quiet pandemic’ of airway issues we’re seeing in modern populations, with reduced jaw sizes and constricted airways that contrast with historical anatomical data showing larger jaw sizes in earlier human populations.
Dr Alfi emphasized the evolutionary shift towards smaller jaws due to changes in diet and lifestyle and highlighted the need for a comprehensive approach in modern orthodontics that considers airway health alongside traditional metrics.
“The entire upper airway, which is so critical for breathing and oxygen and sleep, has become an issue. We also know that this is a huge problem because the majority of adults in this world have obstructive sleep apnea or sleep disordered breathing.”
The role of interdisciplinary treatment planning
Using a workflow that brings together specialists in several disciplines is something that is part of our DNA at DSD. Daniel and Dr Alfi reflected on the possibility of creating a plan that shows virtually all possibilities and the role of interdisciplinary planning when it comes to helping other specialists, the patient and the dentist to ‘see what you see’.
"It takes a team, for sure (…) We need these supportive procedures and treatments. For me, especially if you think about the Mamba mentality, you want the specialists, the professionals that handle each component individually, and our general dentist. And the list goes on and on. We have ENTs on our team, functional medicine doctors, all specialists from dentistry itself. And then what we can do digitally is - especially what we have at DSD - is an ability to integrate all those components in one picture and one software and engineer a fully optimized plan."

Can orthognathics be minimally invasive?
Daniel shared that in his experience planning thousands of cases, many should ideally involve orthognathic - but that in most cases, not only the patient but other colleagues see it as something too complex. Dr Alfi explained the role technology has played when it comes to simplifying jaw surgery and recovery for patients.
“Most of my double jaws from start to finish, incision to closure, are going to be under 60 minutes. And even with a genioplasty or expanded maxilla, if we're doing a three piece double jaw and a genio, we're getting 90 minutes, an hour and a half case, even for the more complicated procedures.
But the reason that I'm able to do that is not because I'm fast as an operator: I understand the technology. I helped pioneer the technology, but I understand it well and I've been using it now for six years, fully custom, and the workflow is completely different. It is less invasive. It utilizes technology and optimizes the efficiency of the procedure by utilizing the information and the technology.”
And can orthognathics be minimally invasive?
“That's an interesting thing, Daniel, about invasiveness, because it's not only the invasiveness of the procedure itself, the direct procedure, because that in and of itself is less invasive because of the custom guides. In place of technology, we can avoid a lot of external scars and incisions, because everything we can do inside the mouth now, which makes that less invasive because of the technology we have.
But also, you're right, stretching somebody's tissues, soft tissues for 8 hours versus stretching for 1 hour, it's a lot less traumatic. So there's much less inflammatory response afterwards.”
What does science say?
To round off the interview, Daniel asked Dr Alfi about clinical evidence: how much can we do to solve this quiet pandemic by expanding and when do we need to go to orthognathics?
“I think that as for any provider that has access, any patient or provider has access to this technology and surgery, for me, it makes more sense to do that in one procedure and get it done, rather than turning for months, then fixing and getting a marginal improvement in airway compared to what we can get with MMA. That's my opinion on it. The problem is an accessibility issue.”
Listen to the episode in full
To hear more from Daniel Ramos and Dr David Alfi on all the issues discussed in this episode, subscribe now on Spotify or Apple Podcasts to listen to the full conversation and stay up to date with upcoming episodes.
About the episode guest
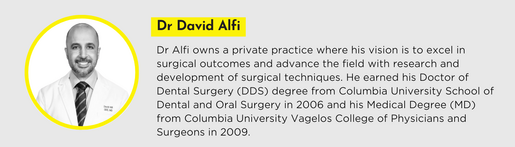
About the host