By Christian Coachman
⋅ 11 min read
⋅ Updated Jun, 2024
FACT: A lot of dentistry is still left to chance.
It’s true that as an experienced clinician it’s perfectly possible to deliver great work for our patients without pre-planning a procedure and being guided by it during the execution. However, it’s also true that this is difficult to do in a consistent and predictable way, leading to inconsistent results which cause dentists, dental teams and patients an immense amount of stress.
We believe that just as an airplane pilot is guided by a meticulous flight plan, with systems and checks in place to ensure perfect execution, dentists and patients should be able to rely on the same type of certainty when it comes to treatment execution and outcomes. And the way to do this is guided dentistry.
To explore how guided dentistry can change the way we think about and perform dental procedures to benefit us and our patients, in this article we will examine an indirect restoration case to examine how a standard and digitally guided method compare in terms of time, cost, stress and patient satisfaction.
If you believe that guided dentistry is too expensive or time consuming - or that the advantages are not worth changing your methods for, this article is for you.

Indirect restoration case comparison: Standard vs. digitally guided method
Data acquisition
Smile design
Treatment planning
Patient treatment presentation
Restorative planning
Reduction guides
Quality control guides
Post-preparation impression
Provisionalization
Final restorations
Quality control
Result
Repairs or repetitions

Discover for yourself the impact guided protocols could have on the predictability and efficiency of your clinical execution with our Guided Dentistry Certification.
1. Data acquisition
Standard
In a standard method of patient data collection there is no systematic and optimized protocol. This can increase the time spent by clinician and patient and impact negatively on the patient’s experience.
Digitally guided
A standardized and optimized information gathering protocol ensures the efficient use of time as well as a positive patient experience.

2. Smile design
Standard
In a standard approach, there is often no prior smile design or 2D smile design.
When the upper alone is designed, we don’t know how this relates to the lower; if you want to analyze the upper design in relation to the lower model, this requires taking a record with the articulator. It is difficult to obtain precise information or truly integrate the smile with the face.
Usually when you order a diagnostic design, it is completely additive and for the upper only. As a result, dentists are not able to really analyze the design and create a treatment plan with this information; everything is additive and you can’t see the impact of the design on the lower arch, so we can’t take care of function.
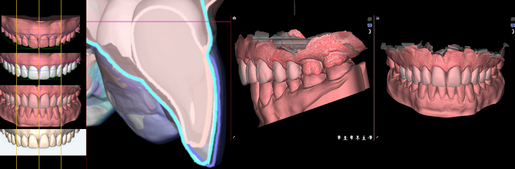
Digitally guided
In a digitally guided approach, the smile design is created in 3D and guided by the patient’s face. This enables us to see the real integration of the smile design with the face and incredibly precise information. Using digital impressions we have the upper and lower as well as the correct occlusion, and when the lab designs the upper we can easily see how this design will impact the lower.
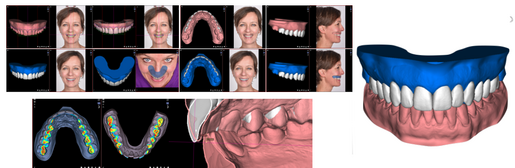
The digitally guided smile design is a tool that helps us start to think straight away about a design that is possible and realistic: we are thinking about esthetics, function and biology, and we can do this because we have all the information we need.

3. Treatment planning
Standard
Decisions are made based on the information from the wax-up (if it has been carried out) and the experience and skill of the clinician. Communication can be less than ideal due to a lack of accurate information and in-person interaction.
Digitally guided
Decisions are made based on being able to see the final result at the beginning of the process. This allows us to predict possible problems and create a realistic treatment plan with a predictable result.
Using digital, we can also take advantage of being able to treatment plan alongside others by communicating asynchronously and using images.

4. Patient treatment presentation
Standard
Patients find it difficult to understand the treatment offered by looking at plaster models or mannequins. Not having a lot of educational information to show a patient about their case can reduce the chance of them accepting treatment.
Digitally guided
Showing the patient an educational presentation which contains images and videos from the 3D planning of their case can increase their perceived value of the treatment and the likelihood of them accepting treatment.

5. Restorative planning
Standard
The clinical treatment is 100% guided by the experience, skill and decisions of the clinician. Most decisions are made during the execution of the treatment.
Digitally guided
Carrying out detailed digital planning for restorative clinical execution allows for better visualization and decision making. This includes treatment suggestions, the location of finishing lines, the type of restoration, strategies, etc.

6. Reduction guides
Standard
Usually there are no reduction guides. When it comes to calibrated preparations, these are made using a motivational mock up which is not a faithful copy of the final result. In many cases the motivational mock up is thicker than the final situation which means that even when we follow the process perfectly - scanning very accurately, calibrating the burr precisely, etc. dental labs will frequently request modifications to preparations because there is a lack of space.
The decision on the amount of prep is subjective and is dictated by the experience and expertise of the individual clinician.
If a guide is used, this is created based on the motivational mock up. As a result, even if we attempt to do everything as perfectly as possible, using this as our starting point means we still receive requests for modifications from the lab.
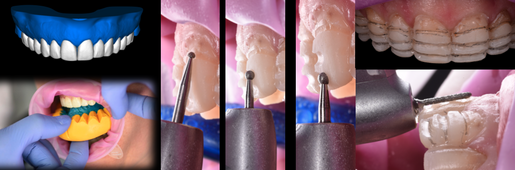
Digitally guided
Using an ideal design which is a faithful copy of the expected final result, we can design and manufacture high-precision reduction guides to prep the exact amount required for the case. This avoids repeated requests for modifications by dental labs.

7. Quality control guides
Standard
Quality control guides are not often used. When they are used, they are generally made on the basis of a model that is not a copy of the final result. This adds inaccuracies. In addition, they are made of flexible silicone which can alter the precision of measurements.
Digitally guided
3D printed quality control guides are designed digitally with high precision, using the final result design as a starting point. They take into account the different faces of the tooth as well as finishing lines.

8. Post preparation impression
Standard
Working in a 100% analog way with impressions leads to a high probability of incorrect impressions. It is also necessary to consider that there may be possible lab failures when developing the different models that can affect the precision of the result or mean that additional appointments are required for corrections. The difficulty of achieving a perfect result with traditional impressions can mean that the lab will adapt their design and cause a lot of back and forth between lab and dentist.
If an intraoral scanner is used, there is usually a lack of quality control systems for the preparations. Again, this can affect the lab result or mean that additional appointments are required for corrections.
Digitally guided
Being successful with intraoral scanning involves implementing standardized protocols to avoid bringing patients back for extra appointments and achieve maximum precision and effectiveness.

9. Provisionalization
Standard
In the standard way of working this can be done either directly or indirectly. However, both ways are usually a copy of the motivational mock up or the patient’s situation prior to the restorations, which is very different from the final expected result.
If we take as an example a case that is not 100% additive, the lab can make another non-additive wax-up. However, in this situation it is difficult to resemble the mock up wax-up and, because there are no control guides, we risk not having enough space to place it.
Digitally guided
Like in the standard way, provisionals can be done directly or indirectly. However, in both cases they will be a copy of the final design produced digitally. This guarantees that the provisional will be very similar to the final restorations.

10. Final restorations
Standard
If done by injection, the lab needs to create a new wax-up on the preparations model that tries to follow the initial and provisional design as closely as possible.
If the restorations are done by stratifying ceramics, they must almost start from scratch and attempt to reproduce the design that the patient approved, taking into account that any small modification has the potential to affect the esthetics, function or biology of the case.
The skill of the technician is paramount in this way of working and the process is laborious.
The benefit of this process is being able to create a truly unique result by mixing colors but if something happens to a product it can be very difficult to redo and replicate it.
Digitally guided
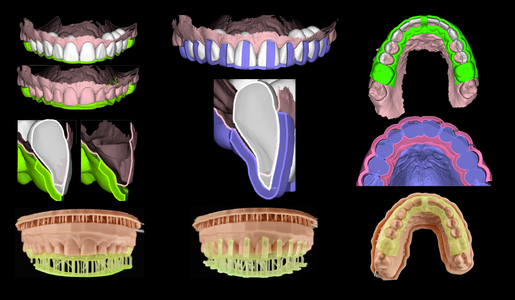
The lab carries out a step which we call ‘DSD over the prep’. This is where the design that the patient approved will be overlapped to the model after prep. It is adapted from the design to the finishing lines and follows the possible adjustments made in the provisionalization phase.
This design is the same as the one the patient approved but with minor adjustments. This significantly reduces the need for design alterations, time spent manufacturing, and the overall dependence on the skills of the dental technician. The process increases the predictability of the result and the similarity of the result to the initial approved design.

11. Quality control
Standard
Very often there is no official quality control. If there is, this is normally done by assessing whether the dentist and the patient are happy with the result. Who is right? This is very subjective and is based on the experience and expertise of the clinician.
Digitally guided
We can carry out a precise quality control by overlapping the ideal design with the digital model of the dental preparations. All measurements can be done with high precision.

12. Result
Standard
In the standard way of working we can certainly obtain a result very similar to the one proposed to the patient, but not in a consistent or predictable way. There are many factors that can alter the result during the process and it might take many appointments to achieve the expected result.
Digitally guided
In most cases the result will be predictable and consistent with no surprises. What we plan will be what we obtain - this is copy-paste dentistry.

13. Repairs or repetitions
Standard
If something goes wrong or fails, it can take many steps or tests to obtain a result that is similar to the original one.
Digitally guided
In a guided way of working, having quality control systems in place makes it easy to identify the problem to correct. As we still have the digital files from each of the steps in the original process, it is easy to repeat a part of the manufacturing process and maintain a standard of quality equal to the original.
When the patient has an issue, being able to solve it in an accurate, predictable and quick way is one of the main benefits of digital.

How would you solve this?

| Digital | Standard |
|---|---|
| Remove | Remove |
| Intraoral scan | Take a new impression |
| Milling | Articulator mounting |
| Bonding | Wax-up |
| New ceramic layering | |
| Test & adjustments | |
| Fine-tune | |
| Bonding |
Learn more about Guided Dentistry
For over 15 years, we have been developing protocols which prove that quality dentistry doesn't need to be stressful or unpredictable.
If you would like to explore how guided procedures could become part of your daily practice, giving you confidence and certainty in clinical execution, check out our Guided Dentistry Certification and explore topics such as:
Course 1: A new approach to dentistry
Course 2: Why guided is non negotiable
Course 3: Increasing predictability & efficiency with devices
Course 4: How to improve restorative cases with guided